Post Bariatric Hypoglycemia (PBH)
Obesity is a disease of global epidemic proportions. The excessive accumulation of adipose tissue accompanied by chronic, systemic inflammation can be associated with the development of numerous co-morbidities (hypertension, type 2 diabetes, cardiovascular disease, dyslipidemia, sleep apnea, orthopedic conditions, some types of cancer, etc.). According to the World Health Organization, more than 2.1 billion adults were estimated to be overweight (1.5 billion) or obese (640 million).
Bariatric surgery is an accepted surgical treatment for obesity in many adults. Bariatric surgery has proven to be highly effective in these subjects, leading to significant improvements in body mass index and obesity-related co-morbidities. The two most common types of bariatric surgeries are the Roux-en-Y (RYGB) and sleeve gastrectomy (SG), and account for approximately 80% of all bariatric surgical procedures.
Bariatric surgery is becoming increasingly used as a treatment for obesity. The most recent IFSO Worldwide Survey (Angrisani et al., Obesity Surgery 2018) reported that 634,897 bariatric operations were performed worldwide in 2016. According to the American Society for Metabolic and Bariatric Surgery, there were 256,000 bariatric surgery procedures in the United States in 2019 alone. This is an increase of almost 60% since 2011. Europe is the second largest market for gastric bypass with 78,677 procedures in 2014 with expected growth to 114,770 by 2020. While Asia remains a smaller market for gastric bypass with approximately 32,266 procedures in 2014, it is the fastest growing market and was expected to reach 90,164 procedures by 2020, for a CAGR of 16.8% between 2015 and 2020.
Many patients that have undergone SG and RYGB procedures display altered postprandial glucose homeostasis. Pronounced postprandial elevations in both plasma glucose and insulin are observed compared to subjects that have not had bariatric surgery. While this is a common observation in post-bariatric subjects, a subset of these subjects develops post bariatric hypoglycemia (PBH).
PBH is a form of reactive hypoglycemia that usually presents 6 months to 4 years post-surgery and is caused by increased circulating glucose and a resulting uncontrolled spike in insulin, typically 1-2 hours after a meal. Symptoms can include those associated with neuroglycopenia such as weakness, drowsiness, dizziness, confusion, seizure and loss of consciousness that can dangerously impair normal day-to-day activities and can sometimes be life-threatening.
First line therapy for PBH patients is limited to significant dietary restrictions that are often ineffective. There are no therapeutics approved for the treatment PBH.
The two graphs below show time course measurements of postprandial circulating blood glucose and insulin in healthy subjects, bariatric surgery patients without PBH, and patients diagnosed with PBH.
Healthy patients that have not undergone bariatric surgery exhibit a normal increase, plateau, and gradual return to normal level of circulating blood glucose and insulin. This typical pattern is represented by the blue lines in the graphs below (Control). Bariatric surgery patients that do not have PBH (Asymptomatic-RYGB) typically experience rapid absorption and elevated levels of circulating glucose. In response, these patient’s body’s secret an elevated, yet moderately controlled increase in insulin coupled with an accelerated return to normal fasting levels when compared to Control. These patients may experience certain symptoms associated with PBH but have not been formally diagnosed with PBH. Patients diagnosed with PBH, represented below by the red line (PBH-RYGB), typically demonstrate the same rapid increase in glucose absorption, but their corresponding secretion of insulin is uncontrolled, leading to postprandial hypoglycemic events.
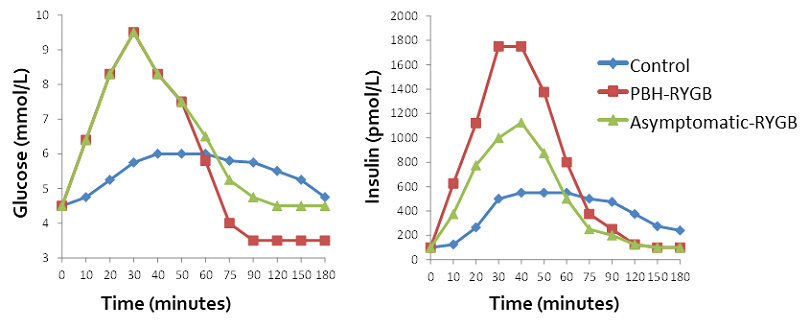
Changes in Post-Prandial Blood Glucose and Insulin Levels in Bariatric Surgery Patients, PBH Patients and Healthy Subjects.
Post bariatric surgery patients, with and without PBH, experience pronounced increases in postprandial blood glucose and insulin compared control. Blue line: Control (healthy subjects); Green line: Asymptomatic-RYGB (Patients that have had RYGB bariatric surgery but do not have PBH; Red line: PBH-RYGB (Patients that have had RYGB bariatric surgery and have been diagnosed with PBH). Reference: Salehi M, Gastaldelli A, D’alessio DA. Altered islet function and insulin clearance cause hyperinsulinemia in gastric bypass patients with symptoms of postprandial hypoglycemia. The Journal of Clinical Endocrinology & Metabolism. 2014 Jun; 99(6): 2008-17.
Changes in Post-Prandial Blood Glucose and Insulin Levels in Bariatric Surgery Patients, PBH Patients and Healthy Subjects.
Post bariatric surgery patients, with and without PBH, experience pronounced increases in postprandial blood glucose and insulin compared control.
Blue line: Control (healthy subjects); Green line: Asymptomatic-RYGB (Patients that have had RYGB bariatric surgery but do not have PBH; Red line: PBH-RYGB (Patients that have had RYGB bariatric surgery and have been diagnosed with PBH).
Reference: Salehi M, Gastaldelli A, D’alessio DA. Altered islet function and insulin clearance cause hyperinsulinemia in gastric bypass patients with symptoms of postprandial hypoglycemia. The Journal of Clinical Endocrinology & Metabolism. 2014 Jun; 99(6): 2008-17.
